Dr. Selby
June 14th, 2021
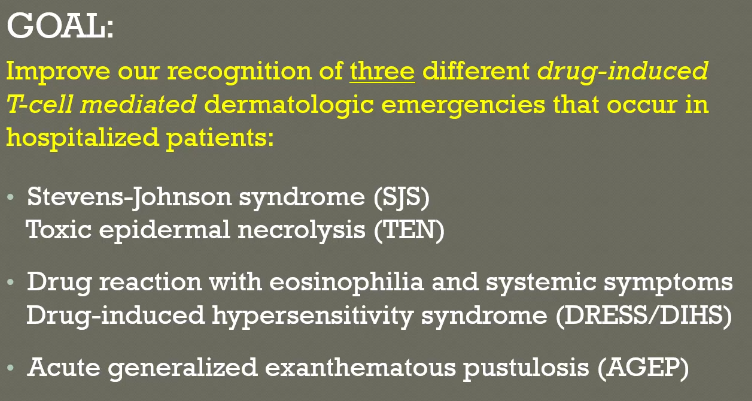
Three big things should be on your radar, especially high yield for boards.
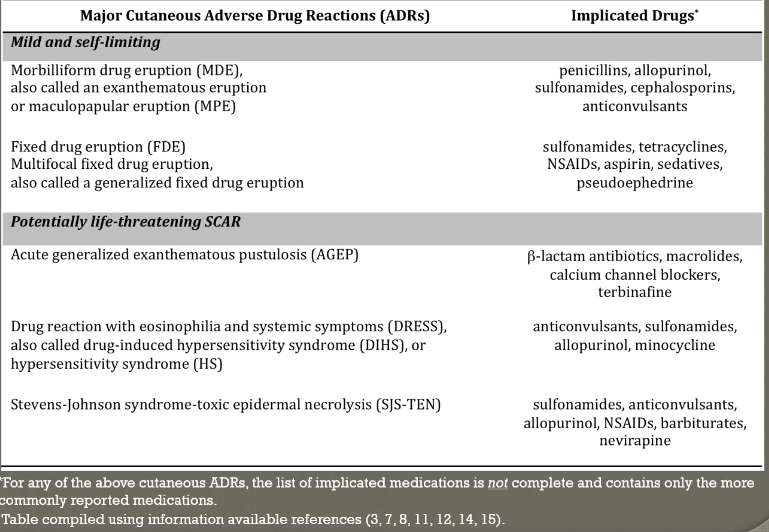
90 % of drug reactions or morbilliform or fixed drug-eruptions and are not a big deal. Self-limited, benign, no acute treatment needed
Overview: Severe reactions are important because they can be life threatening
-
Need to know the high yield drugs for these reactions
-
Need to know the timeline
-
Need to know appearance of the rash and the associated signs and symptoms
Common Drugs
Timelines…

Very boards savy to know. AGEP is very short 1-4 days, classically 48 hours.
Pathophysiology
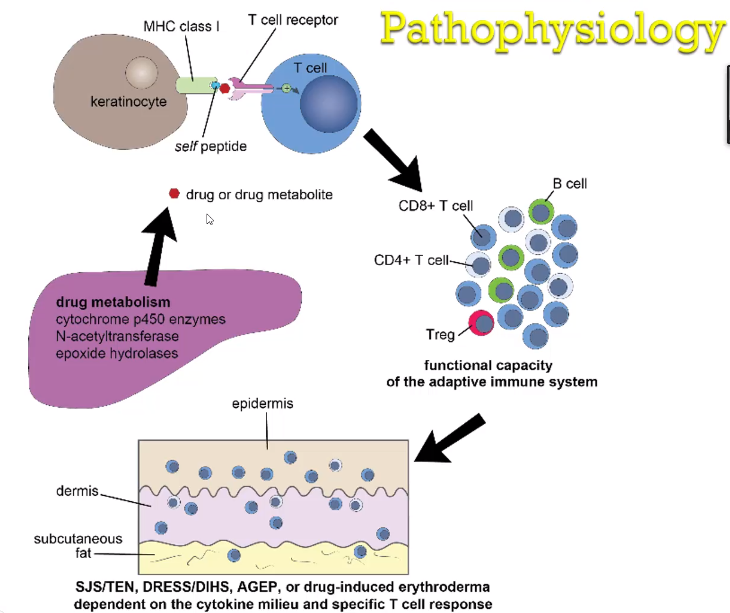
Start in the liver – pharmacologic metabolism starts the process
If the drug metabolite alters a naturally occurring MHC class 1 peptide, the T cells from the body may react and cause self-harm. The T-cell takes the self peptide to the lymph node and generates an adaptive immune response which manifests on the skin. Patients with more robust immune systems will show a more robust drug response. Immunocompromised are less likely to have severe reaction
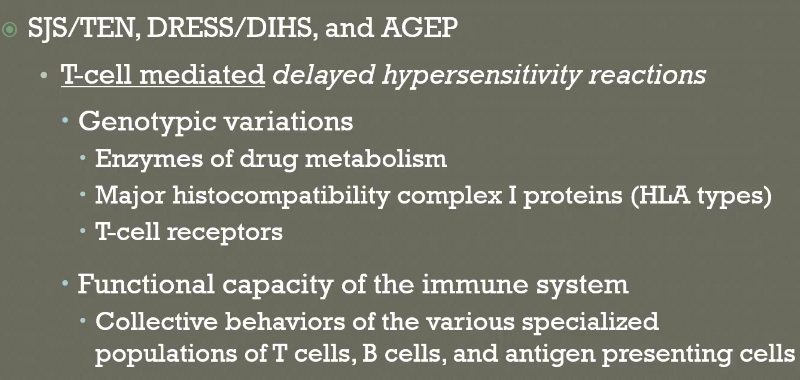
Not immediate, there needs to be time for the immune system response.
Clinical appearance of the rash is determined by the cytokine milieu and the specific T cell response.
SJS / TEN
-
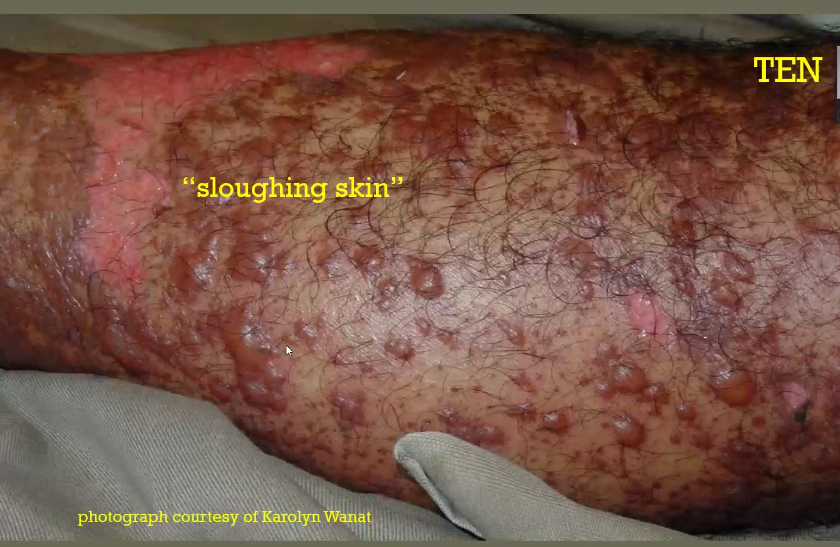
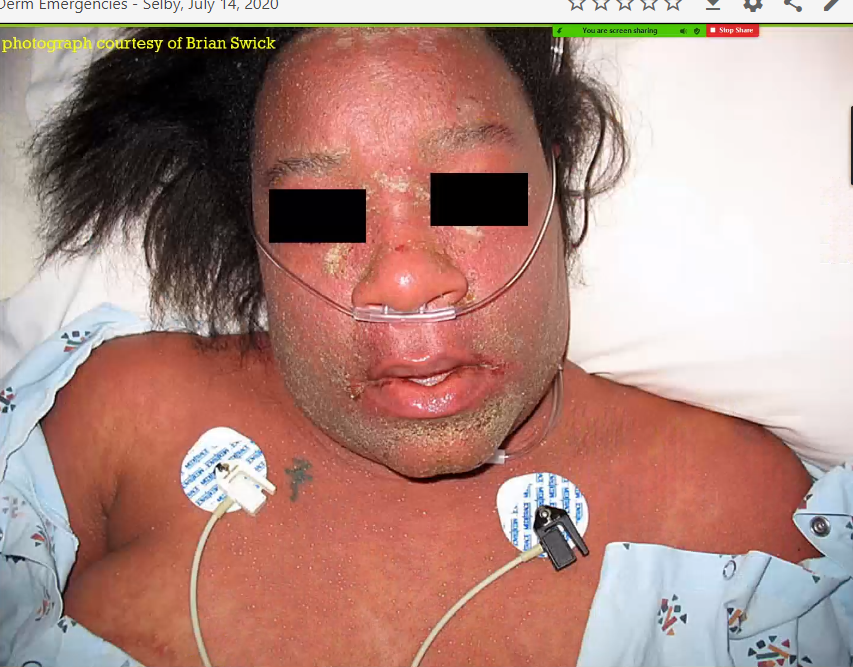
Ultimately an example of TEN. 90% need involvement of 2 mucosal surfaces. Mouth and eyes here are both involed. His nasal mucosa is also involved. Dusky red macules which are the start of epidermal detachment. Starts centrally. Zoomed in pictures show dusky red. It will blanch, blanching is a matter of how much blood is flowing out of the skin and whether you can tamponade it off by pressing on it. Truncal predilection, dusky red coloration, severe mucosal involvement. Epidermal detachment. Sloughing skin, epidermis coming off and you see the dermis.
-
Mucosal involvement
-
Progrome 1-3 days prior to rash: faver, malaise, myalgia
-
SKin rash develops 7-21 days following expousre
-
Bacterial sepsis results from loss of skin
Risk Factors:
Certain MHC classes, slow acetylator phenotypes, Immunocompromised status (HIV/AIDS)
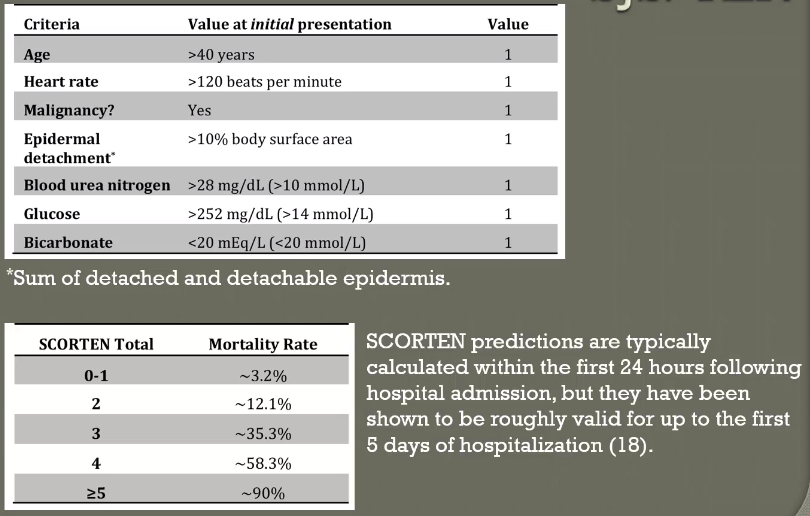
Prognostic criteria SCORETEN: Model validated up to 5 days of hospitalization
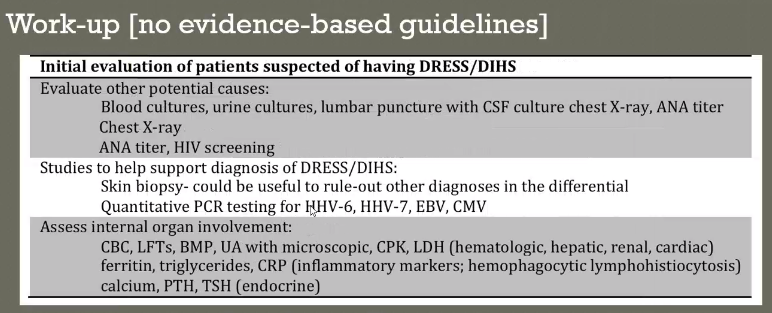
Work Up
Skin biopsy
Detailed timeline of drug exposure of culprit drug
NO DEFINITIVE LAB TEST,
Biggest thing to do is stop the culprit drug which fits and started 1-2 weeks prior
No evidence basded guidelines for adjunctive therapies – (cyclosporine, IVIg, Steroids, TNF inhibitors)
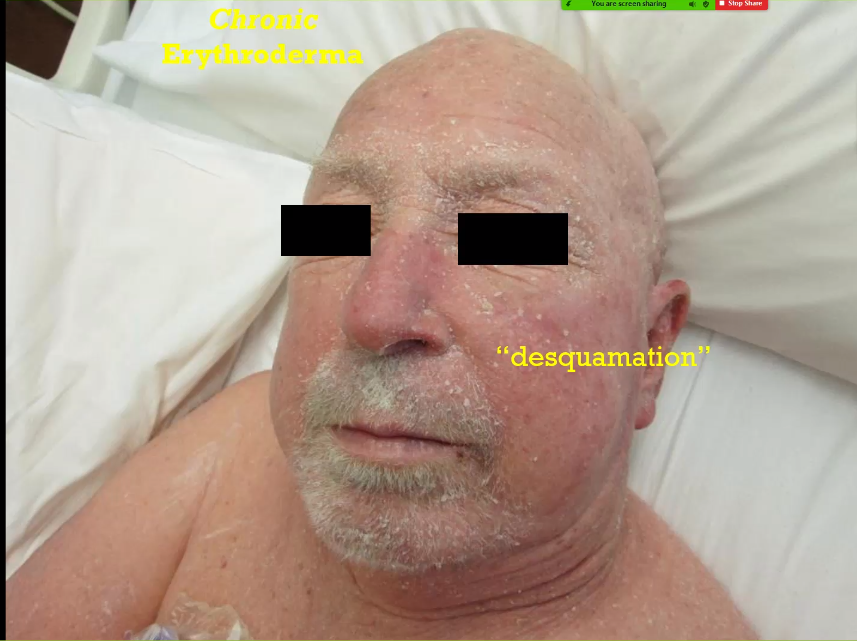
Contrast that with sloughing skin which looks like this. This is desquamation. Just top layer or epidermis. Very different from sloughing skin
Positive Nikolsky Sign – Move thumb to the side and disrupts the epidermis.

Biopsies are never diagnostic, they can support clinical diagnosis.
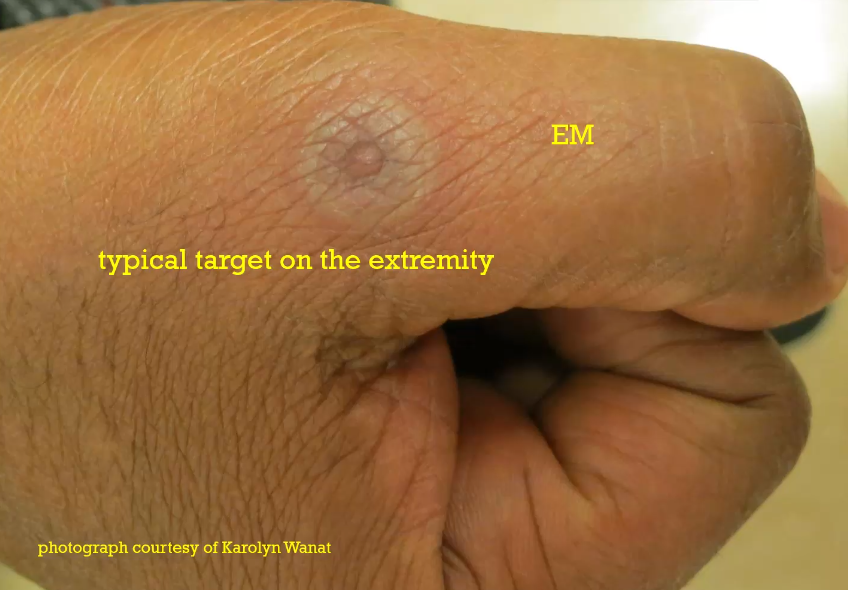
Erythema multiforme is difficult sometimes to distinguish between SJS/TEN because it also has mucosal involvement. Big difference is the targetoid lesions in EM and that it starts on the periphery first then moves to the truncal area unlike SJS which starts in the trunk. Rash is much more ill defined in SJS/TEN.
EM – distal on extremities which are targetoid
Biopsy – cannot tell the difference
EM – distinct disease triggered by infection versus SJS / TEN – caused by drugs
Morbilliform Drug Eruption MDEs
-
Usually not painful, usually itchy. (TEN is very painful)
-
MDEs have no signs of active or impending epidermal detachment (nikolsky negative)
-
MDE is not associated with prodrome or fever
AGEP
Superficial white pustules. Classically starts in the armpits or the groins. Looks like redness from far away, looks like pustules when you get up close.
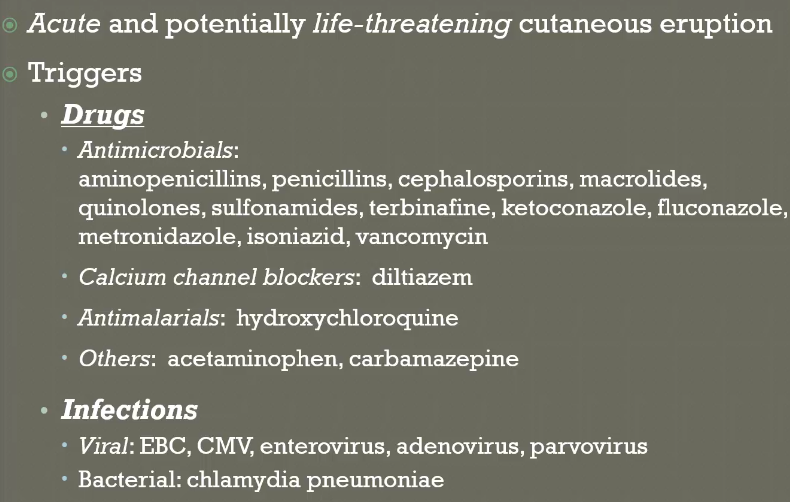
Aminopenicillins, Diltiazem, macrolides are biggest offenders but all antibiotics can do it. Some infections but its usually drugs
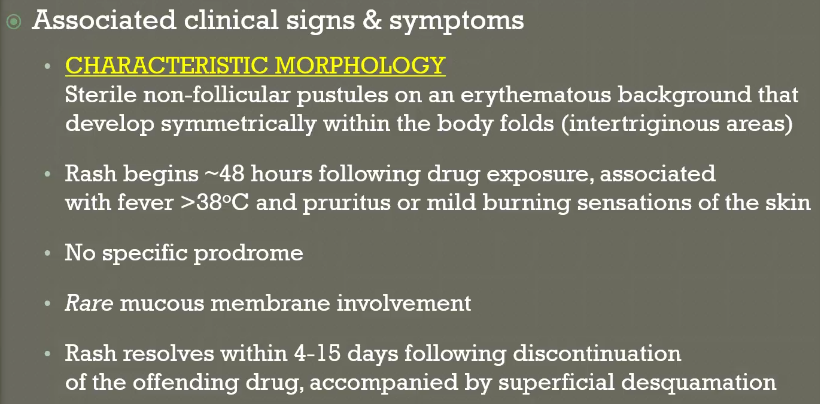
Have to see pustules – usually in armpits and groins first
No mucus membrane involvement
48 hours!!! Desquamation afterwards but no sloughing skin.
Usually stops rapidly after the drug is stopped.
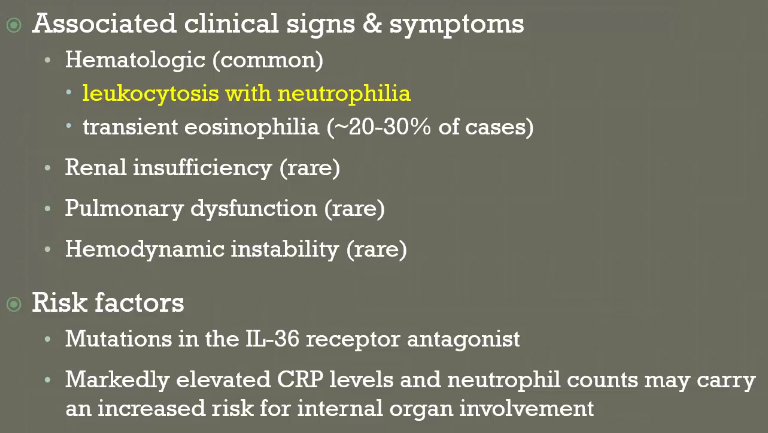
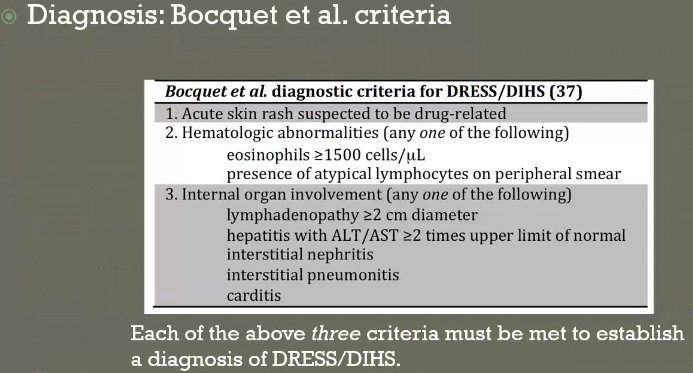
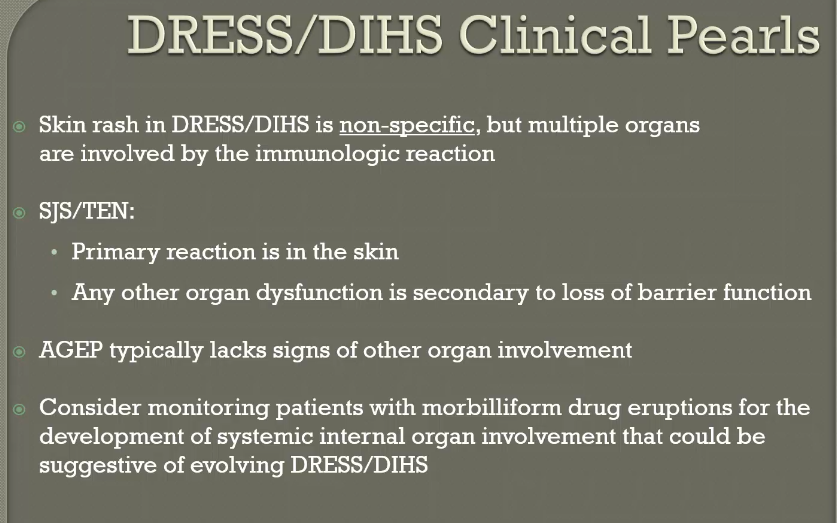
DRESS / DIHS
THIS RASH CAN LOOK LIKE ANYTHING!! Morbilliform eruption on the trunk. Dependent areas appear darker red. Lots of facial and neck redness. Lymphadenopathy is always present. Hands can have targetoid. Dark puple vasulitis type rash. Can look pustular. Timeline is very long, allows time for desquamation.
Main difference between DRESS and SJS is that DRESS has organ involvement, not just skin involvement. T cell mediated organ damage
Dreug reaction with eosinophilia and systemic symptoms. Eosinophilia is not always present.
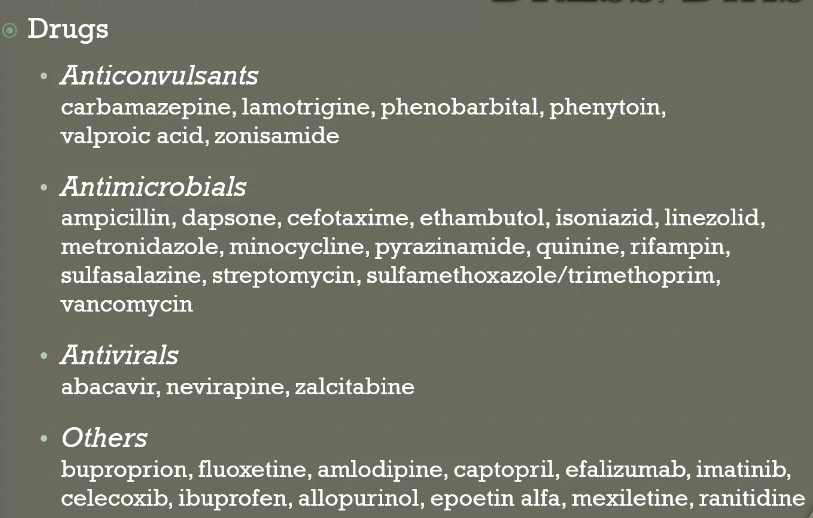
Highlight bactrim and anticonvulsants. Also minocycline.
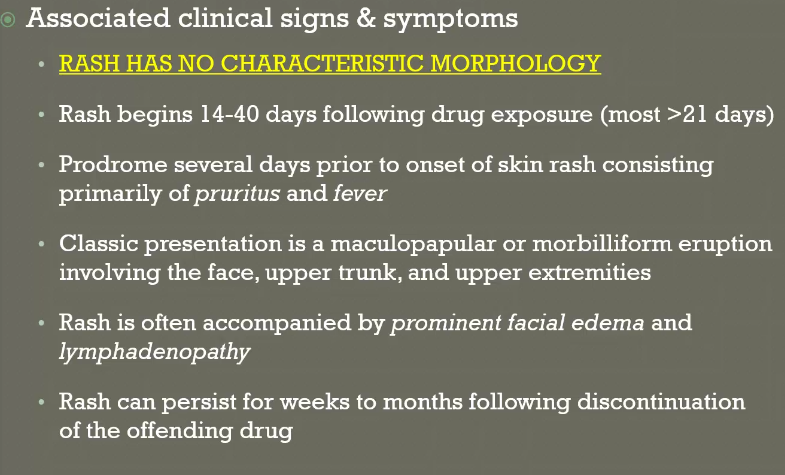
Timeline is much longer than other rashes. Textbook looks like morbilliform but the timeline is much longer.
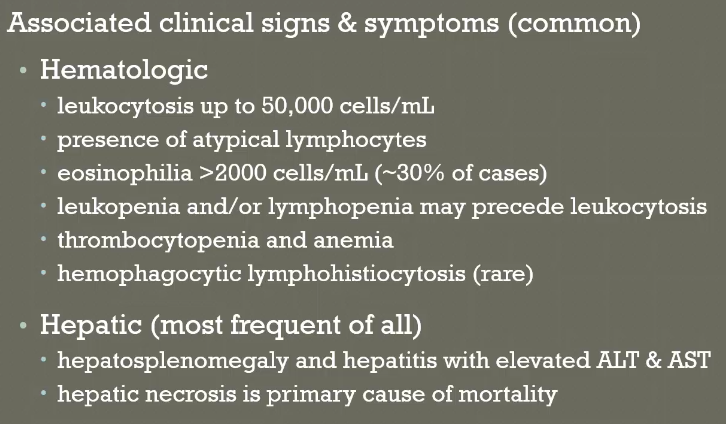
Liver involvement is the most common. AST/ALT. Hepatic necrosis is associated with higher mortality. Hematologic also very common. May see atypical leukocytes on peripheral smear.
Less common: Renal, pulmonary, cardiac
Least common: Neurologic, gastrointestinal, endocrine

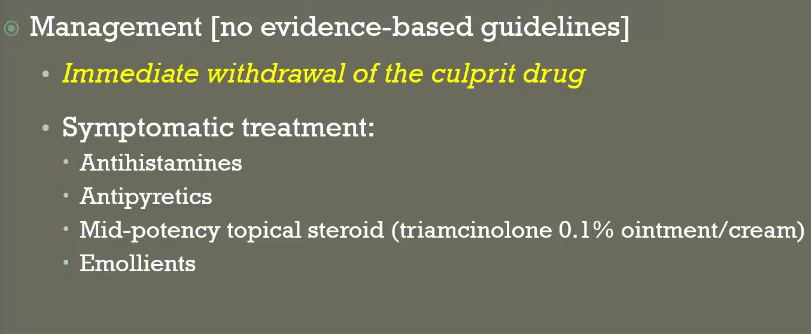
DRESS Management:
Immediate withdrawal of the culprit drug
Systemic steroids dosed 1 mg/kg/day; gradual taper over 3-6 months – different than others
Symptomatic treatment
Antihistamines
Mid-potency topical steroid (triamcinolone 0.1% ointment)
Other immunosuppressive agents are used, nothing evidence based.
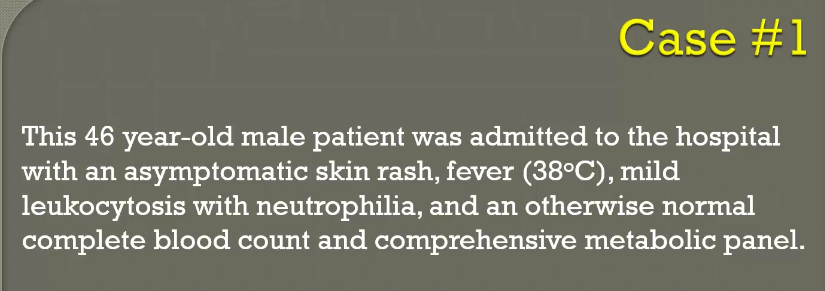

Case 1: Patient has AGEP. Short timeline. Answer is A.

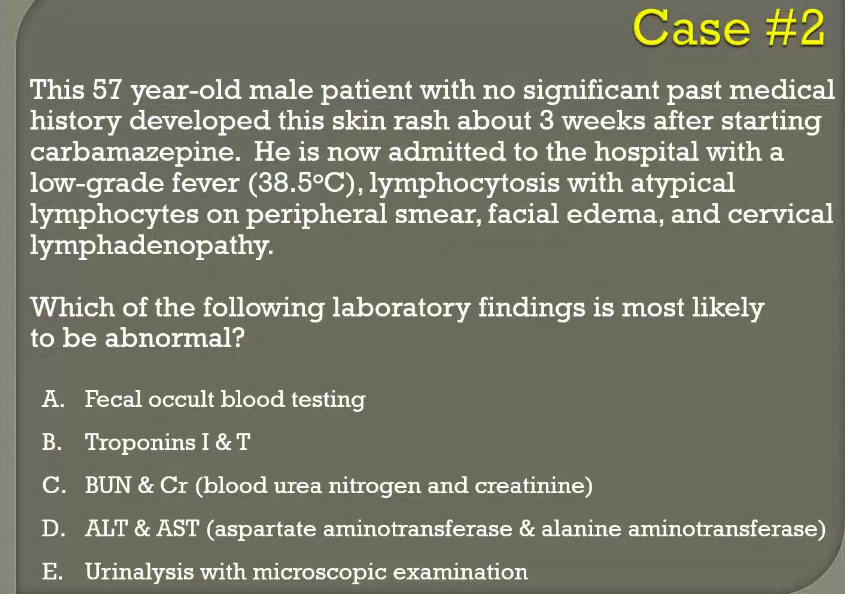
This is a patient with DRESS syndrome
Answer is liver involvement, C


Yes, you can biopsy. It will provide supporting evidence. But the answer is none of the above.
Key Points:
-
Erythema multiforme (EM) can be recognized by the target lesions; a drug or infection (herpes simplex virus or Mycoplasma pneumoniae) can trigger EM.
-
Stevens-Johnson syndrome and toxic epidermal necrolysis are potentially lethal because of widespread skin inflammation, necrosis, and erosion; the two syndromes are distinguished by the amount of skin involved.
-
Drug reaction with eosinophilia and systemic symptoms is a systemic drug hypersensitivity reaction that presents with new rash and flu-like symptoms.
-
Patients with suspected drug hypersensitivity syndrome, also known as drug reaction with eosinophilia and systemic symptoms, should have a complete blood count with differential to evaluate for eosinophilia or atypical lymphocytosis and liver chemistry tests to assess for evidence of systemic organ involvement.
Post by Roger Struble