R2 Talk Handout–Drug-Induced Kidney Injury
Drug Induced Acute Interstitial Nephritis
1. Definition and Prevalence
a. A decline in renal function characterized by inflammatory infiltrate in interstitium brought about by a drug
b. Accounts for about 15-27% of AKIs
2. Culprits
a. NSAIDs
b. Antibiotics
c. Proton Pump Inhibitors
d. Diuretics
e. Allopurinol
3. Presentation
a. Often asymptomatic
b. Can also present with general malaise, nausea, vomiting
c. Classically described as fever, rash, arthralgias
4. Lab Findings
a. Elevated creatinine
b. Eosinophilia
c. Eosinophiluria is less reliable
d. Urine: WBCs, RBCs, white cell casts
5. Diagnosis
a. Definitive diagnosis can be made with renal biopsy
b. Histology shows interstitial edema and infiltrate consisting mostly of T lymphocytes and monocytes
6. Treatment
a. Stop offending agent
b. Follow-up creatinine to ensure resolution
c. Steroids are controversial as no randomized control trials
d. Generally, if discovered early enough and significant inflammation, treatment with steroids is warranted
Most Common Offenders
1. NSAIDs
a. Most frequent cause of drug-induced AIN and renal insufficiency after AIN
b. Bland presentation
c. Often has concurrent nephrotic syndrome
d. Histology: blunting and effacement of foot process and increased glomerular permeability
e. Less responsive to steroids
2. Penicillins
a. More associated with classic triad: fever, rash, arthralgias
b. Histology: allergic and hypersensitivity reactions
i. More prominent eosinophils, can also have hypersensitivity granulomas
c. Better response to steroids
3. Proton Pump Inhibitors
a. Sneakier presentation: <50% fever, <10% rash, <33% develop eosinophilia
b. Histology: classic interstitial inflammation, intact glomeruli
c. Often diagnosed late in course
d. Associated with chronic interstitial fibrosis and development of CKD
i. One study found 20-50% higher risk of CKD
References
-
Moledina DG, Perazella MA. Drug-Induced Acute Interstitial Nephritis. Clin J Am Soc Nephrol. 2017;12(12):2046–2049.
-
Praga M, González E. Acute Interstitial Nephritis. Kidney Int. 2010; 77:956.
-
Prendecki M, Tanna A, Salama AD, et al. Long-term outcome in biopsy-proven acute interstitial nephritis treated with steroids. Clin Kidney J. 2017;10(2):233‐239.
-
Praga M, Appel G. Clinical manifestations and diagnosis of acute interstitial nephritis. 2018. UpToDate.
-
Kshirsagar A, Falk R. Treatment of acute interstitial nephritis. 2019. UpToDate
-
Clarkson, M.R., Giblin, L., O’Connell, F.P. et al. Acute interstitial nephritis: clinical features and response to corticosteroid therapy. Nephrol Dial Transplant. 2004; 19: 2778–2783
-
Pusey CD, et al. Drug associated acute interstitial nephritis: clinical and pathological features and the response to high dose steroid therapy. Qj Med. 1983;52:194-211.
-
Moledina DG, Perazella MA. Proton Pump Inhibitors and CKD. J Am Soc Neph. 2016; 27:2919-2928.
-
Lazarus B, Chen Y, Wilson FP, et al. Proton Pump Inhibitor Use and the Risk of Chronic Kidney Disease. JAMA Intern Med. 2016;176(2):238‐246. doi:10.1001/jamainternmed.2015.7193
-
Kodner CM, Kudrimoti A. Diagnosis and management of acute interstitial nephritis. Am Fam Physician. 2003; 67:2527-2534.
-
Galpin JE, Sinaberger JH, Stanley TM et al. Acute interstitial nephritis due to methicillin. Am J Med 1978; 65: 756–765
-
Porile JL, Bakris GL, Garella S. Acute interstitial nephritis with glomerulopathy due to nonsteroidal anti-inflammatory agents: a review of its clinical spectrum and effects of steroid therapy. J Clin Pharmacol. 1990;30(5):468‐475.
-
Schwarz A, et al. The outcome of acute interstitial nephritis: risk factors for the transition from acute to chronic interstitial nephritis. Clin Nephrol. 2000; 54:179-190.

Alick Feng MD
Urticaria
Background:
– 15-25% will experience at some point
Mechanism:
– IgE mediated from Mast cells and basophils
– Located everywhere: superficial dermis, deep tissues, bone marrow, blood
– Typical immediate symptoms mediated by the following:
o Histamine, heparin, tryptase, cytokines
Description:
– Typical qualities:
o Raised
o Erythematous
o Blanchable
o Pruritic
o Temporal (<24 hours)
o Migratory
o Central Pallor
Classification:
– Acute:
o Less than 6 weeks
o Typical causes:
§ Medications
§ Viral illnesses
§ Foods
§ Contact allergens
§ NSAIDs
§ Opiates/narcotics
o 50% unknown cause.
– Chronic:
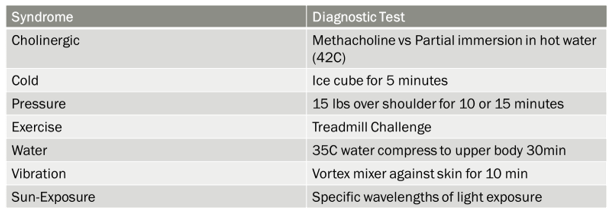
o Physical/inducible urticarias
§ Heat, cold, pressure, exercise, water, vibration, sun exposure
o Chronic Spontaneous Urticaria
§ If not above etiology, the possibly IgG mediated.
§ Related associated autoimmune disorders
· SLE
· RA
· T1DM
· Sjogren’s
· Celiac’s
· Thyroid
Counseling:
Luckily, majority (86%) of patients with chronic spontaneous urticaria resolve within 5 years when no angioedema is there.
Clinical Questions:
– Frequency, timing, duration, pattern of recurrence:
o Differentiate acute vs chronic
– Potential triggers:
o Help with etiology/cause in acute and chronic urticaria (can ask exposures from list and table above)
– RED FLAGS: REQUIRE FURTHER WORK UP
o Lesions > 48 hours
o Fever
o Bruising/left over skin discoloration
o Joint inflammation
– Work up per above:
o Given associated autoimmune disorders, cater labs to appropriate symptoms
o If doing extra labs, have a reason for the lab (I.e., try to restrain from rheum bomb)
§ E.g: If joint inflammation, then can work up for rheumatological cause: ANA, ESR, CRP. Specific antibody testing if more suspicious for SLE or RA. UA and micro for other organ involvement.
o Bruising/left over skin discoloration, longer lasting lesions:
§ Can be associated with hepatitis and associated cryoglobulinemias, HIV, malignancy, vasculitides such as urticarial vasculitis. Rheumatological causes. Adult-onset Still disease, Schnitzler’s syndrome
o Fever:
§ As per above, can be nonspecific for vasculitis and other causes.
Treatment:
First line: Second generation antihistamines. Can be graduated to 4 fold of original dose ( 2 pills in AM, 2 pills in PM)
Burst of prednisone 40mg for severe episodes for approximately 5-10 days reasonable with taper after is reasonable but many may recur if severity is high as you taper.
If above fails and difficult to control, consultation should be considered.
Sources:
Antia, Camila, et al. “Urticaria: A Comprehensive Review.” Journal of the American Academy of Dermatology, vol. 79, no. 4, 2018, pp. 599–614., doi:10.1016/j.jaad.2018.01.020.
Kanani, Amin, et al. “Urticaria and Angioedema.” Allergy, Asthma & Clinical Immunology, vol. 14, no. S2, 2018, doi:10.1186/s13223-018-0288-z.
Spickett, Gp, and C Stroud. “Does This Patient with Urticaria/Angioedema Have Anaphylaxis?” Clinical Medicine, vol. 11, no. 4, 2011, pp. 390–396., doi:10.7861/clinmedicine.11-4-390.
Toubi, E., et al. “Clinical and Laboratory Parameters in Predicting Chronic Urticaria Duration: a Prospective Study of 139 Patients.” Allergy, vol. 59, no. 8, 2004, pp. 869–873., doi:10.1111/j.1398-9995.2004.00473.x.
