Dr. Alejandro Comellas.
Division of Pulmonary and Critical Care
Basics on Mechanical Ventilation
July 2020
Dr. Paul Nassar
Ventilation Management
Division of Pulmonary and Critical Care
2017


Fundamental Concepts
Invasive mechanical ventilation refers to the administration of ventilation directly in the trachea via an endotracheal tube or tracheostomy.
1. Breath control: This refers to the method by which the mechanical breath is delivered. If the tidal volume and inspiratory flow are designated, the breath is classified as volume controlled (VC). Conversely, if the breath is delivered based on a preset inspiratory pressure, the breath is pressure controlled (PC).
2. Breath sequence: Spontaneous and mandatory are the two types of breaths. A mandatory breath is started (triggered) or ended (cycled) by the machine; ventilators may also be set to allow triggering of a mandatory breath coordinated with patient inspiratory effort. If the breath is both triggered and cycled by the patient, it is a spontaneous breath. By definition, a mandatory breath is always assisted (that is, the machine does some portion of the work of breathing), but a spontaneous breath may or may not be assisted. Therefore, there are three breath sequences:
-
Continuous mandatory ventilation (CMV): All breaths are mandatory. A preset frequency represents the minimum number of mandatory breaths per minute; the patient may trigger breaths at a higher frequency.
-
Intermittent mandatory ventilation (IMV): Spontaneous breaths are allowed between or during mandatory breaths. A preset frequency represents the maximum number of mandatory breaths per minute.
-
Continuous spontaneous ventilation (CSV): All breaths are spontaneous.
-
Titrate the ventilator settings to acceptable physiological parameters (i.e., some degree of hypoxemia and hypercapnia is okay.
-
Use low tidal volumes to avoid ventilator-induced lung injury.
-
Use the lowest fraction of inspired oxygen (FIO2) to maintain oxygenation at 90%-92%. Positive end expiratory pressure (PEEP) can recruit collapsed lung units and improve oxygenation.
-
Note: If the patient’s respiratory status acutely decompensates or the ventilator is sounding an alarm or malfunctioning, you can always disconnect the patient from the ventilator and manually ventilate with a bag valve mask while you troubleshoot.
Patients should be assessed daily for their readiness to be weaned from mechanical ventilation by withdrawing sedation and performing a spontaneous breathing trial.

Modes of mechanical ventilation. There are two basic methods. Volume or pressure.
Volume mode – you are setting the volume. This is the standard volume that will be delivered. Continuous mode can only be used when a patient is paralyzed, the patient is not allowed to trigger. Assist control is usually what is used in the ICU. You deliver a set rate, if a patient wants more volume, they are allowed to trigger breathes and receive the set amount of volume.
Pressure mode, you are delivering a set rate of pressure. The patient is then allowed to breath a variable amount of volume depending on the lung compliance and patient demand for carbon dioxide exchange. The rate is usually not set, but there is a backup rate.
Volume control is used at our ICU because it protects the patient from barotrauma, or damage to lungs from added pressure and lung distension. This is very important for patients with COVID and ARDS. You deliver a safe amount of volume at an increased rate.

Minute ventilation is established by the patient. The patient is the one who wants a certain amount of air for gas exchange. The patient will either increase their volume or increase their rate in order to achieve this amount of air. Minute ventilation is volume times rate. We will use sedative medications to reduce minute ventilation in order to protect the patient’s lungs.
Flow: VC the flow is always constant. In pressure, the flow is always variable.
Compliance: The ability of the lung to expand. May be decreased from pulmonary edema, damage to lungs, pneumothorax. If compliance is low, then tidal volume may be lowered. This must always be calculated on each patient
Resistance: Often in the airways. This may be acutely decreased from bronchospasm, mucus plugging, increased secretions.
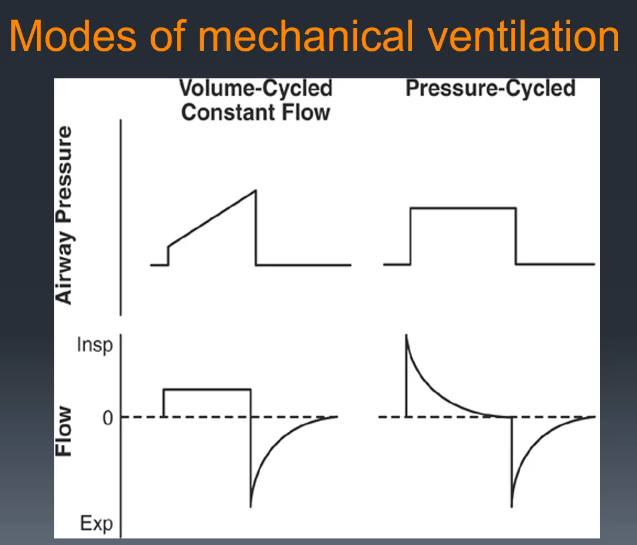
Depending on the mode, one of the cycles will be constant. It looks like a box with controlled delivery.

When the pressure curve reaches its peak, this is the peak pressure.
If you put a pause at the end of inspiration, you measure the static pressure, called the plateau pressure. This is the pressure in the system at that complete tidal volume. You can see the plateau pressure above after the peak, the pressure plateaus to the right.
For pressure cycles, there is no such thing as a peak pressure or plateau pressure, there is a set defined pressure that is given. You have PEEP and pressure support above PEEP on delivered breathes.
PEEP: positive end expiratory pressure. Pressure that is always maintained on the lungs to keep the alveoli open and prevent them from collapsing.

By measuring the peak and plateau pressure, you can determine physiologic characteristics. Airway resistance and lung compliance. Difference between the peak pressure and plateau pressure is the airway resistance. Normal for airway resistance is around 10.
Compliance is calculated based on the tidal volume divided by the difference between the plateau and the PEEP. Normal is around 70 mL of water.
Auto-Peep is calculated from an expiratory hold procedure. The patient is increasing the pressure at the end of exhalation. You will see a rising curve when holding exhalation if auto-peep is present. This may occur in various obstructive airway patterns. Also known as airway trapping. Pressure increases and may be dangerous to the patient.
See the video for some cases!
CHEST GUIDELINES LINK
NEJM VENTILATOR INDUCED LUNG INJURY REVIEW
Post by Roger D. Struble MD MPH
Twitter: @jazzscrubs
