Cardiac Electrophysiology
July 20, 2020
Don Brown EKG Guide

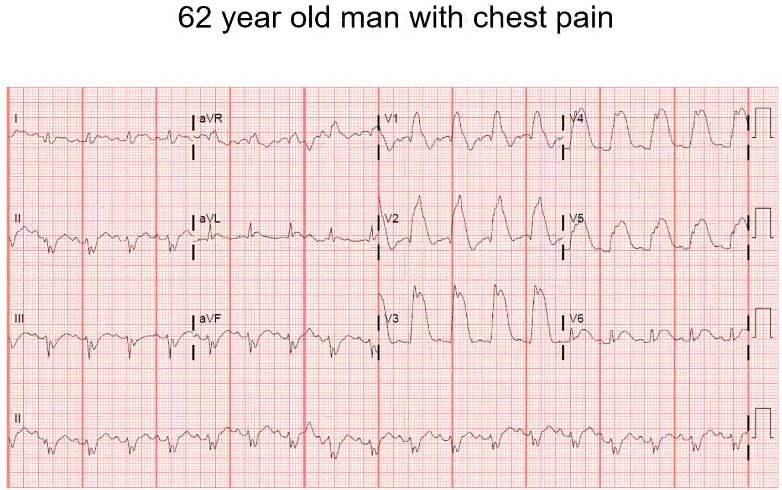
Fast and wide, not consistently. Look at lead 2, QRS is wide and different. Very pronounced in the precordial leads where the QRS has different degress of width. Fast, up to 300 beats per minute on some beats. This patient has pre-excitation, WPW. Probably started in orthodromic reentrant tachycardia (ORT). Know that it is a left sided aberrancy pathway because V1, V2 look like a right bundle branch block. ORT drove him into afib, and once he was in A-fib he started utilizing the accessory pathway, which is high risk because there is no control on the rate like there is in the AV node. The accesory pathway tired out here, stopped conducting and he went through his AV node where he had the three narrow beats.
Do not want to give this patient AV nodal blocking agents. Beta blockade or calcium channel blockers. This will block the AV nodal pathway but not the aberrant pathway.
Want to give procainamide because it is a 1a sodium channel blocking agent which will slow down the AV node pathway and the aberrant pathway.
If the patient is unstable or procainamide is not available, you can cardiovert the patient to terminate the rhythm. Fast, pre-excited afib with one near pre-syncopal episode. This patient was given amiodarone in the field which worsened his rhythm. He was promptly cardioverted when he arrived to the ED.

This rhythm is fast and narrow. All of the QRS are consistent. Do you see any p waves? ….
There may be some retrograde p waves that are visualized in II or III. This patient is in SVT. This is typical AVNRT. There is also a pseudo R prim in V1. It looks like a R prime but in reality it is a retrograde p wave. You also see rate related ischemic changes in lateral leads because of how fast and how long she has been going.
Medication to terminate this rhythm would be adenosine. If you are going to give it on the floor, ask for a 3 way stop cock. You want to give saline afterwards because the half life is so short and you want to be sure that it reaches the target to get an effect. If no effect, you want to be sure drug was actually delivered. Keep 12 lead attached while giving so you can see the rhythm change.

This is how AVNRT gets started. You have sinus rhythm with upright p waves. The T wave deforms because it is acutally a PAC. This conducts slowly down the slow pathway with a long PR. In the time that it takes for the slow pathway to conduct, the fast has recovered and you conduct back up the fast pathway.

Sinus rhythm. Start in the rhythm strip. PR is long, gets longer, and suddenly there is a p wave without a QRS. After the dropped beat we see the next PR is back to normal, and progressively lengthens. Mobitz type I. Inferiorly you can see a STEMI.

In a case like this, you want to spend a lot of time on the rhythm strip. Is there a p wave in front of every QRS? Is there more P’s than QRS’s?
There are more p’s than QRS’s. If you look at the first few beats in the rythm strip you would think it is in 2:1 conduction. But the PR interval is not fixed so 2:1 does not fit. You can see P waves in the QRS, you can see a P wave immediately after the QRS. Recently had a procedure from interventionalist. She is in sinus tachycardia with complete AV block, and junctional escape. Very slow escape rhythm which is very sensitive to ectopic beats, you can see it delayed from the PVC. Remember to use rhythm strip.
Treat with a pacemaker.

Based on this EKG, what do you think may be some electrolyte abnormalities?
Sinus, p wave before all QRS. But the QTc is prolonged. P wave is starting at downslope of the U wave. You can see the “lumpy, bumpy” biphasic t wave into u wave. Hypocalcemia will give you an isoelectric line and then a prolonged QT with a normal T wave. A way to tell the difference between hypocalcemia and hypokalemia. Both can prolong the QT. Hypocalcemia gives you an isoelectric line with a t wave that is pushed out.
Long qt, over 600 miliseconds. Here you can see a R on T phenomenon. Longer R to R before this, QT stretches. Then have a short beat, typically a PVC, hits at susceptible timing when the QT is at its longest. PVC falls on T wave which then initiates Torsades de pointes. Based on this EKG, you should be very concerned the patient has hypokalemia. In addition to potassium, this patient should be given magnesium. You could also speed the patient up and shorten the QT interval. This could be done with isoproterenol or even by putting in a pacemaker wire to overdrive and suppress everything to drive fast.

MWF dialysis patient. Skipped his dialysis session. What electrolyte abnormality do you think of?
Wide, known dialysis patient, potassium was 8-9 on admission.

Sinus rhythm, p in front of each qrs. Both are normal. Notice that the QT is long. In the precordial leads the QT is long and there are T-wave inversions. In a patient found down, something that could explain this EKG is a CNS event (massive stroke), this can give you very impressive global t wave inversions, especially in the precordium. Laterally the QT is usually the longest, here you can see almost 800 second QT intervals.
QRS is wide. You see a RBBB. Is it a typical RBBB? You notice that the RBBB is out very lateral as well. You can see 15 mm of ST elevation. This patient is having an anterior STEMI. Any conduction delay can make a STEMI diagnosis more challenging. In this case you see concordant ST elevation with the QRS. The lateral leads are the most prominent.

Here is what happens with an old LBB and a STEMI. You can still diagnose in the setting of a LBBB. Look at the old EKG. They may have a LBBB but the usually don’t have this degree of ST change.

P wave in front of each QRS. Faster then 100, so sinus tachycardia. QT is on the short side. Money is on the rhythm strip. You can see electrical alternans. Heart is swinging in the pericardial effusion. As it swings away and towards you can see changes in the QRS voltage. Very concerning for large pericardial effusion. You can also see some change in SVTs, but not this significant change in voltage that you see with large pericardial effusion. This is hard to see in any leads other than the rhythm strip.

This is wide and fast. You do not see p waves in front of every QRS. This is a patient with known heart failure, what does that increase his risk for?
You have more V’s that A’s. It has to be a ventricular rhythm. This patient has slow Ventricular tachycardia. He is in a 2:1 retrograde conduction with wide left bundle branch morphology VT with retrograde atrial conduction.
Link to Don Brown’s Pocket EKG Guide and EKG practice website for more learning.
Post by Roger D. Struble MD MPH
