Sydney Bowmaster, MD
Mentor: Kevin Doerschug, MD
Definitions:
· Hospital-acquired pneumonia (HAP): ≥48 hrs after hospitalization
· Ventilator-associated pneumonia (VAP): ≥48 hrs after endotracheal intubation
· Ventilated hospital-acquired pneumonia: HAP patients who later require intubation
Pathogenesis:
· Microaspiration of colonized organisms, usually bacterial and from oropharyngeal site
· Direct contact with contaminated equipment or healthcare personnel
· Inhalation of infectious aerosols
· Typical microbiology:
o Aerobic GNR: Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterobacter species, Acinetobacter species
o GPC: Staph aureus, Strep species
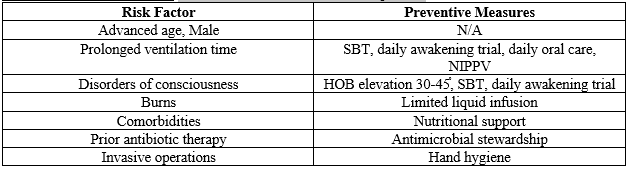
Risk Factors & Prevention: VAP occurs in ~10% of intubated patients
Clinical Features:
· Signs/symptoms: Fever, tachypnea, increased purulent secretions, hemoptysis, rhonchi/rales, reduced breath sounds, bronchospasm, worsening hypoxemia, leukocytosis/leukopenia
· Radiographic findings: new/progressive infiltrate
· Altered ventilator mechanics: reduced tidal volume, increased inspiratory pressures
Diagnosis: New infiltrate + infectious signs + positive culture
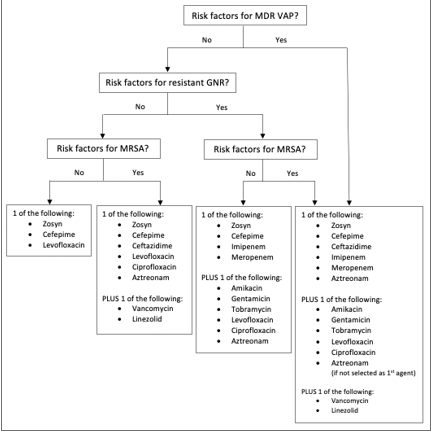
Treatment: (See flowchart below)
· Empiric therapy depends on risk for resistant organisms.
· Risk for MDR pathogens if ANY of these: Septic shock, IV antibiotics within previous 90 days, ARDS, hospitalization ≥5 days, acute renal replacement therapy, structural lung disease (bronchiectasis, cystic fibrosis)
· Risk for resistant GNR: local antibiogram shows that >10% of GNR are resistant to agent being considered for monotherapy, or prevalence of resistance is unknown
· Risk for MRSA: local antibiogram shows >10-20% of Staph aureus isolates are MRSA, or prevalence of MRSA is unknown
· Narrow based on culture & sensitivity results
o MRSA swab has high negative predictive value. Use this to guide de-escalation.
· Total duration of antibiotic treatment: 7 days
Prognosis: Attributable mortality ~13%
· Adequate antibiotic therapy is important!
· Factors associated with poor outcomes: shock, coma, ARDS, high APACHE score, bacteremia, severe underlying comorbidities, infection caused by MDR organism, multilobar disease, cavitating lesions, rapidly progressive infiltrates, delay in effective antimicrobial therapy
References:
1. Berton DC, Kalil AC, Teixeira PJ. Quantitative versus qualitative cultures of respiratory secretions for clinical outcomes in patients with ventilator-associated pneumonia. Cochrane Database Syst Rev 2014; :CD006482.
2. Dangerfield B, Chung A, Webb B, Seville MT. Predictive value of methicillin-resistant Staphylococcus aureus nasal swab PCR assay for MRSA pneumonia. Antimicrob Agents Chemother. 2014;58:859-864.
3. Dominedò C, Ceccato A, Torres A. Ventilator-associated pneumonia: new principles guiding empiric antibiotic therapy. Curr Opin Infect Dis. 2020;33(2):182-188.
4. Garrouste-Orgeas M, Chevret S, Arlet G, et al. Oropharyngeal or gastric colonization and nosocomial pneumonia in adult intensive care unit patients. A prospective study based on genomic DNA analysis. Am J Respir Crit Care Med 1997;156(5):1647-55.
5. Jones RN. Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clin Infect Dis 2010; 51 Suppl 1:S81.
6. Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 2016; 63:e61.
7. Melsen WG, Rovers MM, Groenwold RH, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13:665-671.
8. Mergenhagen KA, Starr KE, Wattengel BA, et al. Determining the utility of methicillin-resistant Staphylococcus aureus nares screening in antimicrobial stewardship. Clin Infect Dis 2019; Epub 2019/10/02. Doi: 10.1093/cid/ciz974.
9. Muscedere JG, Day A, Heyland DK. Mortality, attributable mortality, and clinical events as endpoints for clinical trials of ventilator-associated pneumonia and hospital-acquired pneumonia. Clin Infect Dis. 2010;51(Suppl1):S120-S125.
10. Muscedere JG, Shorr AF, Jiang X, et al. The adequacy of timely empiric antibiotic therapy for ventilator-associated pneumonia: an important determinant of outcome. J Crit Care 2012;27(3):322.e7-14.
11. Sievert DM, Ricks P, Edwards JR, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol 2013;34(1):1-14.
12. Weber DJ, Rutala WA, Sickbert-Bennett EE, et al. Microbiology of ventilator-associated pneumonia compared with that of hospital-acquired pneumonia. Infect Control Hosp Epidemiol 2007;28(7):825-31.
13. Wu D, Wu C, Zhang S, et al. Risk Factors of Ventilator-Associated Pneumonia in Critically Ill Patients. Front Pharmacol 2019;10:482.
